Abstract
Introduction: Erythropoiesis-stimulating agents (ESAs) such as epoetin alfa or darbepoetin alfa (DA) are recommended in current clinical guidelines to treat anemia in patients with low-risk myelodysplastic syndrome (MDS) requiring red blood cell (RBC) transfusion. However, ESAs are not approved in all countries for MDS treatment. A phase 3, placebo-controlled trial was conducted to evaluate efficacy of subcutaneous DA vs placebo in patients with low/int-1-risk MDS and anemia (ARCADE; NCT01362140). In a follow-up companion study (NCT02175277), DA treatment was continued for patients in Belgium. Here, we report results from the companion study.
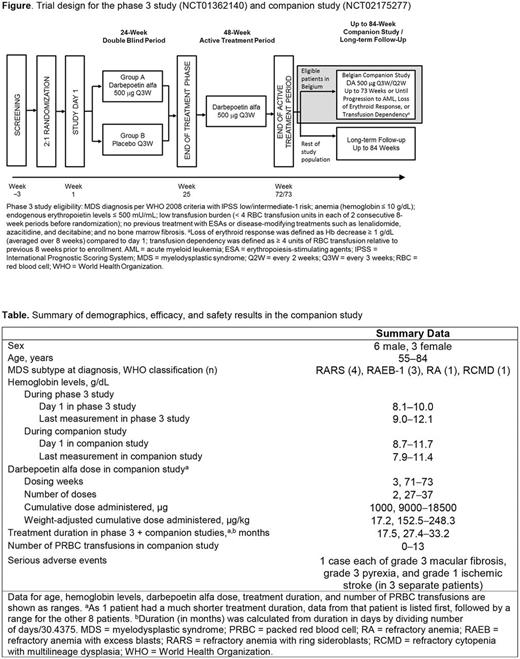
Methods: This was a phase 3b, open-label, single-arm, companion study for the continued DA treatment of patients in Belgium who completed the active treatment period (ATP) of the parent MDS phase 3 study (ARCADE) and had ongoing clinically relevant erythroid response. In the phase 3 study, eligible patients (as described by Platzbecker et al ASH 2016; Figure) had been stratified by IPSS risk (low/int-1) and randomized 2:1 to 24 weeks of treatment with DA 500 µg every 3 weeks (Q3W) or placebo, followed by a 48-week ATP in which all patients received DA 500 µg Q3W. Eligible patients in Belgium were enrolled in the phase 3b companion study to provide required DA access beyond the ATP of the phase 3 study.
Eligibility for the companion study included completion of the parent phase 3 study, ongoing clinically relevant erythroid response at week 70/71 per investigator's clinical judgment, and signing of informed consent. Patients continued DA treatment up to 73 weeks or until progression to acute myeloid leukemia (AML; per WHO criteria), loss of erythroid response (hemoglobin [Hb] decrease ≥ 1 g/dL compared to day 1, averaged over 8 weeks), or transfusion dependency (≥ 4 units of RBC transfusion relative to previous 8 weeks prior to enrollment) (Figure).
The first DA dose in the companion study was the same as that administered at the last dosing visit (week 70/71) in the parent phase 3 study. Investigators could maintain or change the DA dose/frequency depending on erythroid response and the most recent Hb value before each dosing visit (500 µg Q2W max dose). If a patient's Hb reached > 12.0 g/dL, DA was to be withheld until Hb decreased to ≤ 11.0 g/dL, at which time treatment was to be restarted at a reduced dose. DA was stopped in patients requiring ≥ 4 dose reductions. Safety was evaluated throughout the study.
Results: A total of 146 patients were enrolled in the phase 3 study. Of those, 9 patients were enrolled in the phase 3b companion study at 5 centers in Belgium and are included in this analysis. Six patients were male and 3 were female, with age ranging from 55 to 84 years (Table). One patient received 2 DA doses and the other 8 received DA doses ranging from 27 to 37 in the companion study, with treatment duration ranging from 17.5 to 33.2 months over the course of the parent phase 3 and companion studies. Of the 9 patients, 1 had 3 packed RBC (PRBC) transfusions in the month before starting the companion study (ie, in the parent phase 3 study) and 5 patients had PRBC transfusions during the companion study (Table). Patients continued to show an erythroid response, per investigator assessment. Adverse events were reported for all 9 patients and were primarily grade 1-2 in severity. Two patients had grade 3 adverse events (macular fibrosis in 1 patient and hematochezia and neutropenia in 1 patient); no grade 4 or 5 adverse events were reported. Three patients had serious adverse events not considered to be related to DA per investigator (grade 3 macular fibrosis, grade 1 pyrexia, and grade 1 ischemic stroke; Table). One patient developed a thrombovascular event (TVE; grade 1 ischemic stroke lasting 1 day) 4 weeks after inclusion in the study. The TVE was not considered to be due to treatment; however, DA was discontinued. No patient tested positive for anti-DA or anti-erythropoietin antibodies. No deaths or progression to AML were reported during the study.
Conclusions: This was an analysis of 9 MDS patients who were initially enrolled in a large phase 3 study of DA at 5 centers in Belgium. DA treatment for up to 3 years continued to be efficacious, indicating that sustained treatment with DA in patients with low/int-1-risk MDS and anemia results in prolonged responses. No new safety signals and no progression to AML were reported in this study.
Delforge: Amgen Inc.: Honoraria. Vande Broek: Amgen Inc.: Membership on an entity's Board of Directors or advisory committees; Celgene: Membership on an entity's Board of Directors or advisory committees; Jansen: Membership on an entity's Board of Directors or advisory committees, Other: Speaker's fee. Caers: Amgen Inc.: Honoraria, Membership on an entity's Board of Directors or advisory committees. Badre: Amgen Inc.: Employment, Equity Ownership. Mehta: Amgen Inc.: Employment, Equity Ownership. De Oliveira Brandao: Amgen Inc.: Employment, Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal